Living with type 1 diabetes can be a daily struggle for those unable to produce sufficient insulin to regulate their blood sugar levels. But what if there was a groundbreaking solution on the horizon that could potentially transform how this chronic condition is managed?
Imagine a world where individuals with type 1 diabetes could have a long-term treatment option that doesn’t involve invasive surgeries or frequent injections. This vision is becoming closer to reality, thanks to innovative research in the field of 3D printing.
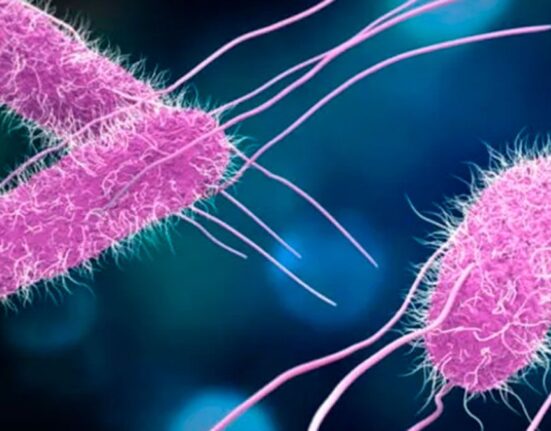
Traditionally, one approach for treating type 1 diabetes involves transplanting human islets – clusters of insulin-producing cells – from donors into patients. However, this method necessitates invasive surgery and poses challenges such as islet functionality loss over time, requiring multiple transplants for sustained effectiveness.
Enter the realm of 3D printing technology, which offers a promising avenue for developing more efficient and less invasive treatments. Researchers are now exploring the use of 3D-printed devices made of live insulin-producing cells that could potentially revolutionize how type 1 diabetes is managed.
Quentin Perrier from the Wake Forest Institute for Regenerative Medicine in North Carolina explains,
“Current practice is to inject these human islets through the portal vein into the liver.”
By utilizing innovative bioink composed of human pancreatic tissue and alginate, researchers are able to create intricate structures that support cell survival and function when placed under the skin.
Adam Feinberg from Carnegie Mellon University emphasizes the significance of achieving high cell density within these printed structures. He notes,
“The higher the density [of islets], the smaller the size of the device you would need to plant in the patient.”
One key advantage of this approach lies in its potential to reduce stress and inflammation on implanted cells, thereby extending their functional lifespan within the body. The porous grid design allows for optimal integration with surrounding tissues, promoting vascular growth crucial for long-term viability.
While these findings show great promise in lab settings, transitioning them into practical clinical applications presents its own set of challenges. Perrier acknowledges this by stating,
“The next challenge is really to validate this finding in vivo.”
Feinberg’s work also demonstrates encouraging results with diabetic lab mice showing restored glucose control for an extended period using 3D-printed islets embedded within hydrogel polymers. Despite acknowledging promising outcomes from current research efforts, Feinberg highlights potential hurdles associated with variability in human tissue used for creating these bioengineered structures.
Looking ahead, both researchers advocate for exploring stem cell therapies as a future frontier in type 1 diabetes treatment through 3D printing technology. By harnessing stem cells during the printing process instead of conventional sources, they believe it could address existing limitations and pave the way for more personalized and effective interventions.
As advancements continue at a rapid pace in merging biotechnology with cutting-edge manufacturing techniques like 3D printing, there’s newfound hope on the horizon for individuals grappling with type 1 diabetes. The prospect of tailored treatments offering sustained relief without major surgical interventions opens up exciting possibilities for enhancing quality of life and redefining standards in managing chronic conditions like never before.
In conclusion, leveraging innovative solutions like 3D-printed insulin-producing cell devices holds immense potential towards creating a paradigm shift in how we approach treating type 1 diabetes. With each scientific breakthrough bringing us closer to tangible solutions that blend precision engineering with biological intricacies, it’s clear that we stand at a transformative crossroads ushering in new horizons for healthcare innovation.




Leave feedback about this